2023 Validation Report
Review for: DisclosedRx
Validation Achieved: Savings
Savings Valid Through: July 2024
Company Profile
Category:
Pharmacy Benefit Management
Website:
Public or Private:
Private
Year Established:
2020
President:
Zack Robinson
Company Contact:
Description:
Everyone should have access to the right medicine, at the right time, at the right cost: and they shouldn’t have to navigate a cumbersome and daunting system to access it.
DisclosedRx’s vision is that truthfulness and innovation will drive greater access to prescription medications for their members at a lower net cost to their client, as well as make them the easiest PBM to partner with.
DisclosedRx offers a fully disclosed pharmacy benefit service to employers. DisclosedRx is contractually obligated to only derive revenue from their clients, allowing them to optimize pharmacy spend without worrying about commitments to the supply chain. DisclosedRx does not earn money by reselling drugs at a higher price than it obtains them (“spread pricing”); it credits all rebates and supply chain credits to the payer; and it charges only one administrative fee. DisclosedRx systems and processes provide claims processing oversight that incorporate active risk management of pharma spend. The risk management programs include mitigation strategies for specialty and high-cost brand medicines. No allegiance to the supply chain allows DisclosedRx to pursue all possible channels for lower cost medications. Payers not only have clear data about their benefits but also gain the advantage of lower costs.
Claim Assertion
DisclosedRx’s Agile Channel Management program applies drug manufacturer copay discounts and patient assistance programs to lower the plan’s expenses. DisclosedRx also uses international sources for certain drugs to deliver a lower cost. Together, these programs reduced a plan’s costs by 32% in a 12-month period.
Method/Calculation/Examples
For each of the three programs – copay discounts, patient assistance programs, and international sources – the analysis compared what the plan would have paid under DisclosedRx contracts (net of rebates) to what the plan ultimately paid. Note: copay programs savings reduced the plan’s costs; member copays may have been reduced or eliminated, but those savings are not shown here.
The patient assistance and international programs had the effect of reducing rebates the plan would have received. These rebates were estimated based upon rebates the plan received in the same time period. The estimated rebates reduced the “Without Disclosed Rx” amounts.
The plan’s total costs reflect estimated rebates for the time period. Rebates were estimated using actual rebates received in the first three quarters of the time period and estimating the rebate for the fourth quarter.
The savings is expressed as a percentage of the plan’s total costs, net of rebates.
Findings & Validation
Table 1 summarizes the three programs and their impact on the plan’s expenses for a 12-month period. 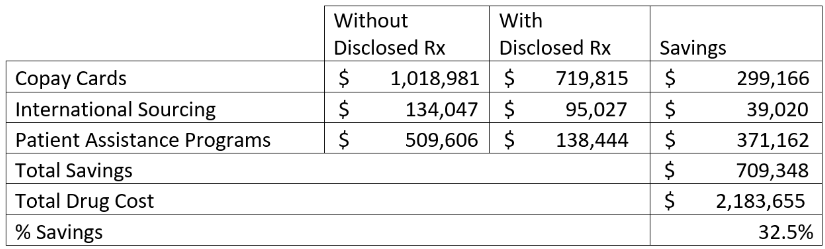
Limitations
Demographics of the plan members were not analyzed, though there is no reason to expect these to vary significantly from the average. Therefore, most employers could expect similar results to the extent the group had similar opportunities for copay discounts, international sourcing, and patient assistance programs.
Validation and Credibility Guarantee
DisclosedRx’s Agile Channel Management program achieved validation for Savings. Validation Institute is willing to provide up to a $25,000 guarantee as part of their Credibility Guarantee Program. To learn more, visit https://validationinstitute.com/credibility-guarantee/.
Program Validation
Program has strong evidence of significant impact on both patient outcomes and on medical costs. Evidence is assessed based upon the certainty it provides that the result is due to the program and not to other factors, such as recruiting people to participate in the program who are most likely to succeed.
Savings
Can reduce health care spending per case/participant or for the plan/purchaser overall.
Outcomes
Product/solution has measurably improved an outcome (risk, hba1c, events, employee retention, etc.) of importance.
Metrics
Credible sources and valid assumptions create a reasonable estimate of a program’s impact.
Contractual Integrity
Vendor is willing to put a part of their fees "at risk" as a guarantee.
About Validation Institute
Validation Institute is a professional community that advocates for organizations and approaches that deliver better health value - stronger health outcomes at lower cost. We connect, train, and certify health care purchasers, and we validate and connect providers delivering superior results. Founded in 2014, the mission of the organization has consistently been to help provide transparency to buyers of health care.
Validation Review ProcessValidation Institute has a team of epidemiologists and statisticians who review each program. The team focuses on three components:
- Evidence from published literature that a similar intervention had similar results.
- The reliability and credibility of the data sources.
- The rigor of the approach to calculating results
To achieve validation, the program has to satisfy each of these components. VI’s team then summarizes the review into a report which is publicly available. Details of VI’s review are available with the program’s permission.